Seven months in, more than half a year since treatment.
I am on Facebook groups related to HSCT: HSCT in Mexico, HSCT in Russia, HSCT in general. The posts in these groups are mostly people considering HSCT at the beginning of the process. They are in the questioning phase, trying to get information, looking for certainty and guarantees where there are none. How much does it cost? What should I bring? Where is the research? Will it work for my specific snowflake of symptoms and diagnosis? How many people had it improve their walking/pain/fatigue…? For how many people did this not work? Did you regret it? Reaching for hope and afraid of the future no matter which choice they make.

Many will never make it happen – because of fear, because of money, because of family demands, because it just isn’t right, because they are not willing to face disappointment, etc.. I was there, I remember how that felt. I had all the same questions, though I did do a better job of searching the page history before asking a question that had already been asked over and over. I trolled the comment threads. I read through the files. I dug up the research – less research than I wished there was. I wanted stone-cold guarantees and clarity. I ultimately had to find my way to make the choice inside the discomfort of ambivalence.
And then I did it. I went to Mexico. I spent a full month there. I went through treatment that was simultaneously hard and brief. I spent the money. It is done, in the rearview mirror. Now the calendar is back to spinning forward faster and faster and when I look in that rearview mirror, the memory of that time is fading fast.
After I got home, I followed the blogs, private Facebook groups, and Instagram pages of people who were in the cohort right behind me. I paid close attention to their journeys, and I had personal connections to some. The next month came, and I paid a little less attention, the next month even less. Now I am no longer following the stories. I pop into the FB groups of people asking the questions at the beginning and answer things where I can, where others haven’t already answered the same questions a million times over.
I am currently in a Facebook group of people who have completed the treatment with the questions we all ask now. How long did you feel this way? When did things change for you? How long was your roller coaster? What did you do to get through it? We are all looking for stories that match ours, for a string to hold onto out of the maze. There are many for whom this time is now far in the rearview mirror. They pop in less and less to offer stories and advice. For now, I am of the ones asking the questions, seeking stories that match my snowflakes self. There will come a time when this phase is in the rearview mirror for me as well.
Legs/walking:
These days I am feeling stuck in pain. Spasticity is a bitch. It seems to be getting harder, even though I felt like it was as hard as it could get already. I hope, I trust. I hope, I trust. I hope, I trust? that this is just a tunnel to get through. I have to believe that. These are still early days, 7 months into a recovery arc that lasts up to 24 months for some. However, when I live in this body day by day, each day can feel eternal and the next seven months inconceivable.
Occasionally there are moments where I feel like I could dance. These moments come out of nowhere. I don’t know what causes them and I don’t know how to re-create them. But they arrive and give me hope; if my body can do this at all, it’s capable of doing this more. The connections aren’t lost. The structure, the skeleton of movement, is there waiting to be released. These teaser moments are a gift. Water in the desert. They take my breath away. They are joyful. They are too brief.
In the meantime I continue to do physical therapy, massage therapy, cardiovascular exercise to the best I can, and the MSgym. My goal, my mission, is to keep that skeletal under structure strong and resilient for when the spasticity eventually subsides.
The Mollii Suit
A woman from the UK, who is about two months behind me and dealing with the same degree of spasticity/spasms, recently posted a photograph of herself in what looks like a wet suit.

It turns out it is a rehabilitation apparatus full of electrical impulses, “functional electrical stimulation”, called the Mollii Suit.
“What is the Mollii Suit?
The Mollii Suit (formerly Elektrodress) is a functional garment that consists of a pair of trousers, a jacket and a detachable control unit which sends electrical signals to the user via electrodes on the inside of the garment. Mollii is an assistive device that people with muscle stiffness (spasticity) or other forms of motor disability can use in their home environment. It can help to reduce undesired reflexes and stiffness, thus enabling an improved posture, range of motion and functional ability. It can also reduce certain types of pain and improve sleep patterns.
How does it work?
The suit has 58 electrodes which can be combined in various ways. Mollii has a control unit which is individually programmed for each user. The person prescribing Mollii uses a computer program to adapt the active electrodes and the intensity (which muscles are to be activated by means of current). The settings are then saved in the Mollii control unit making it simple for the device to be used at home. Mollii uses low level electric current to produce basic tension in the musculature. The current stimulates the antagonist to the spastic muscle. If, for example, the biceps is spastic, the tricep is stimulated which in turn makes the biceps relax. Relaxing the muscle enables active movement and a gradual improvement in function. The physiological mechanism is called reciprocal inhibition.
Who can benefit from using it?
Mollii can be used by adults and children with neurological conditions such as multiple sclerosis, cerebral palsy, acquired brain damage, spinal cord injury and stroke. Mollii provides tailored rehabilitation in the form of a garment with electrotherapy programmed according to the individual’s requirements.”
This woman reported that after a short time wearing the suit it greatly relieved her spasming. The relief doesn’t last forever, but it is meaningful relief that can be repeated. This suit is not available in the fucking US because of the fucking FDA. Even in the UK, on the NHS, I don’t believe it is free. At this point, if it worked, I wouldn’t care if it costs something. I want this suit.
Arms/hands:
I’m still not putting my focus here because the spasticity in my legs and the pain in my hips are so on fire. Someone in my online physical therapy group mentioned she noticed she was deferring to her stronger hand/arm because things were getting harder with her affected arm. Because the brain reinforces what you do it every day, through neuroplasticity, she was making it a practice to embrace the struggle and use her challenged arm even though it made things slower and more difficult. Use it or lose it. Challenge accepted.
Fatigue:
Fatigue continues to not be an issue, at least not MS fatigue. I can feel exhausted when my muscles contract all the time, but that is different and hopefully solvable. I don’t have hours or entire days where I just have to lie down and take a nap for no apparent reason like I used to. I’ll take the win.
Bladder:
Ups and downs here. I’m noticing a correlation between increased overall spasticity and increased urgency. Mostly this isn’t a problem. I no longer worry about being out somewhere and having to find a bathroom quickly.
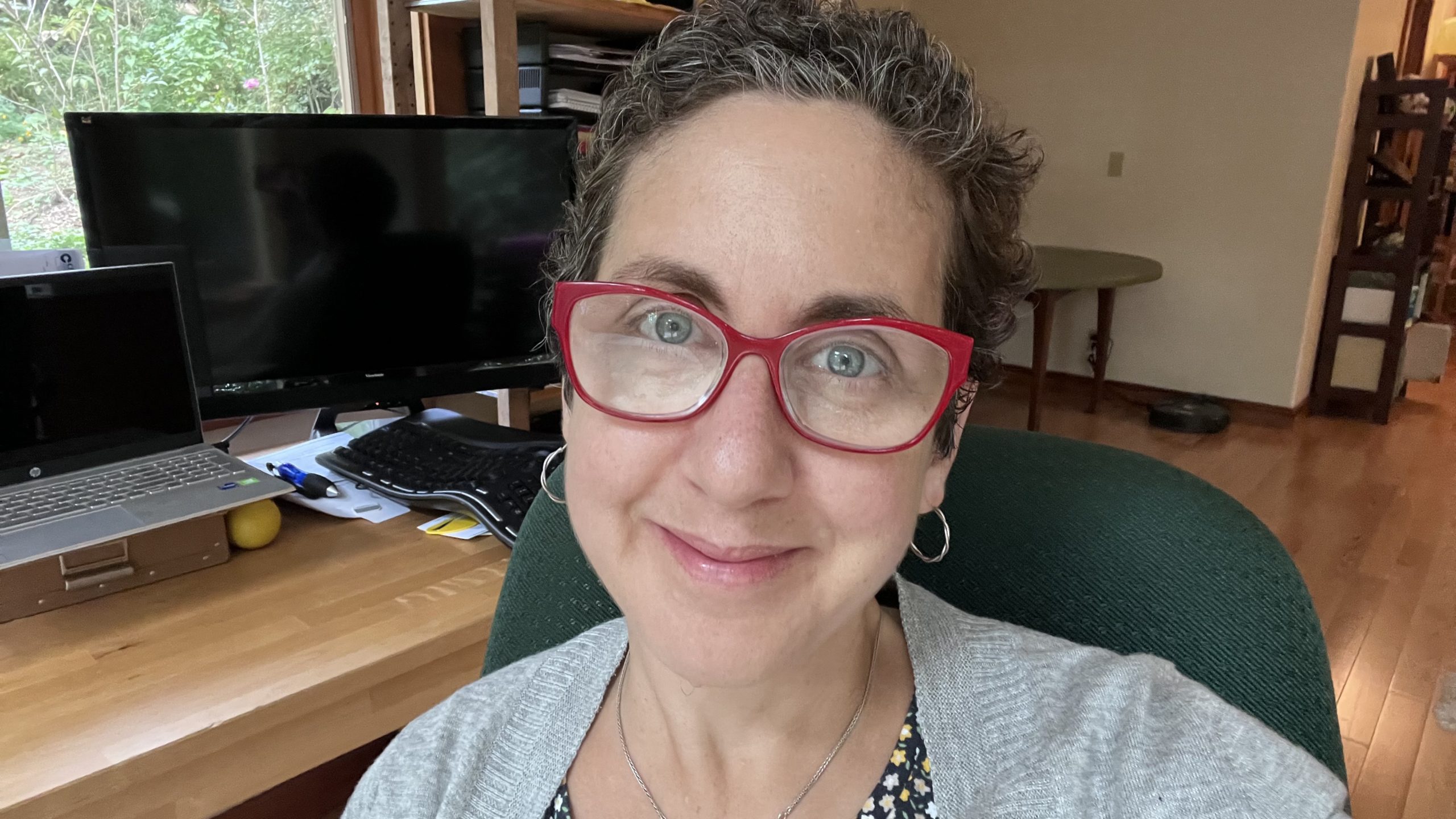
Hair:
A picture is worth the proverbial 1000 words. I will add some words, however. I am reaching the uncomfortable part of growing out one’s hair. Decisions need to be made – stay the course through the awkward growing out phase, or cut it short again and never know what the future could hold. Given how tightly curled my hair is right now, I imagine it will be going up in all directions, for a while, before changing tack and heading south under the weight of gravity. My curiosity for what it will look like after chemo is keeping me from cutting it even though it is so easy short, the practical choice certainly.

Medication:
A lot going on in this category this month. I continue to be on Baclofen and gabapentin at their maximum dosages, I’m not sure they’re making any difference at all. Beginning this week, I am weaning myself off the gabapentin. I am doing this for the most part because I don’t think it’s helping, at least not very much and definitely not enough. I am also doing this because I’m pretty sure it is causing weight gain and digestion woes.
Baclofen, I’m coming for you next! Hopefully this doesn’t screw me over the way it did last time I tried to wean off a medication.
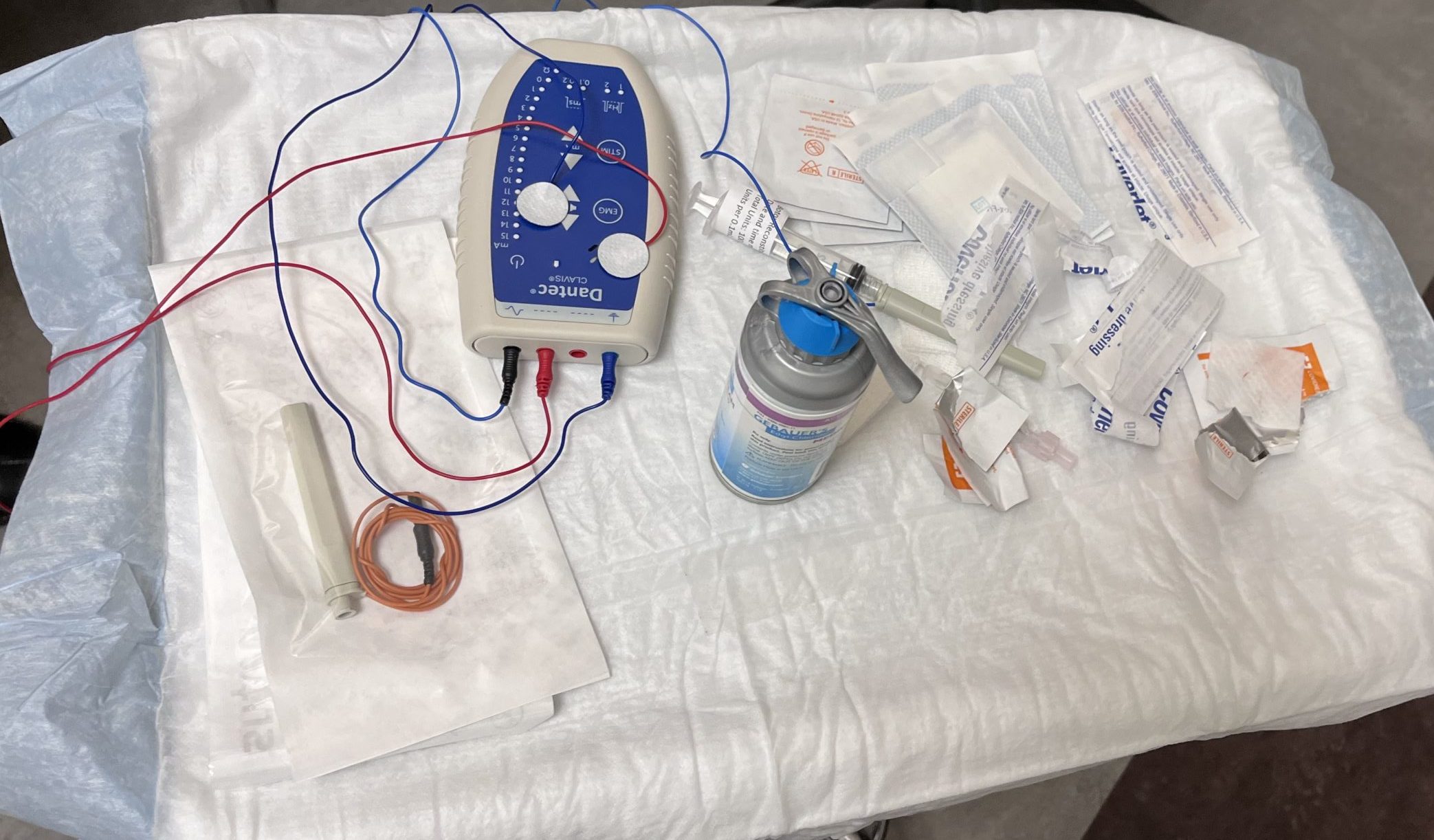
About three weeks ago my physiatrist injected Botox into my right hamstrings and calf muscles to see if that would reduce the spasticity. It can take up to four weeks for this to fully take effect but so far, I’m not noticing anything. It is critical to start low with this medication. Too little and you feel nothing for three months. Too much and your leg is a noodle for three months.
The process of injecting botox into the muscle is fascinating. The practitioner has a device attached to a very thin needle that delivers the botox. The device can “hear” the activity/contractility of the muscle. The practitioner literally fishes around with the needle inserted into the muscle, looking for the highest amount of “sound” the muscle is making and then injecting at this location. It is like standing behind an old television set, adjusting the rabbit ears trying to get the TV signal to come in. Or like moving around the room with your phone trying to get better signal when you are at the limit of the range.

Last week I started taking LDN (low dose naltrexone). According to the National MS Society:
“Naltrexone is an opiate antagonist that is taken orally to block opioid docking sites (receptors) on cells. It is approved by the U.S. Food and Drug Administration (FDA) for the treatment of addictions to opioids and alcohol. At significantly lower doses, low-dose Naltrexone has been used off-label as a treatment for various types of cancers, HIV/AIDS, Parkinson’s disease, Alzheimer’s disease, amyotrophic lateral sclerosis (ALS), emphysema, as well as multiple sclerosis (MS) and other autoimmune diseases.”
I am now at the highest dose possible for this, 4.5 mg per day. The hope for this is decreased pain in my hips and back. So far not noticing any benefit here either. I will give it another couple of weeks.