Hi y’all, it’s been awhile…
It started with a niggling, a little scratch in my throat, the slightest bit of congestion in my nose – my first virus since transplant in February 2022 – one full year virus free. It was a very small virus, nothing at all, barely noticeable. But it tipped my physiologic balance, and I ended up in the emergency room on a Saturday with a UTI allowed to thrive in a disrupted immune system.
The round of antibiotics used to suppress the UTI, to the best of our understanding, shifted my digestive tract into dysbiosis – all the tiny bacteria in my gut, the carefully balanced harmonious communities, lost their song.
Slow motility (constipation by a gentler name) combined with the disrupted microbiome led to SIBO (small intestinal bacterial overgrowth). This is a condition where the bacteria that normally reside, happily and helpfully, in the large intestine get translocated up into the small intestine where they don’t belong. There, the bacteria feast – happy little creatures farting out their metabolic byproducts in someone else’s house. My whole abdomen became bloated and distended, a taut balloon, a pregnant belly with no child joy to offset the suffering. My gut in turmoil triggered my MS symptoms into overdrive – muscle spasms and off-the-charts spasticity.
Here are some quotes from my daily writing practice:
“Who knew that muscles around the torso could create a hug so tight you didn’t want to love anymore?”
“Those of us with MS learn to tolerate by inches by centimeters by millimeters. We normalize discomfort. We normalize living with it.”
“It could be wild rage trying to find its way out. Or maybe wild grief throwing around like a hurricane inside of a small room with no vent out for the circulating wind.”
“It’s the smallest thing – sitting up in the morning, putting my legs and my feet to the floor, considering standing with their persistent rebellion. No one can see it, but it can feel it like an elephant sitting on top of me – that strong, that immense. It looks like nothing from the outside. It’s the smallest thing to others, but it’s an elephant to me.”
In trying to sort this out I have worked with my PCP and undergone colonoscopy prep without the colonoscopy -twice! – trying to empty out the meters of small and large intestine. When that didn’t work, I was referred to a neuro-gastroenterologist – fancy, big title. He was a sweet guy, on the young side, who always wears poop emoji socks when he sees patients. Cute.
By the time I met with him, my PCP and I felt confident that I had SIBO. He agreed that I had “dysbiosis” and prescribed rifaximin, an antibiotic that very specifically targets the bacteria in the small intestine and nowhere else, which insurance doesn’t cover, and is incredibly hard to get. I happened to mention this to a friend and neighbor who had gone through SIBO, and she said, “oh I have a bunch left over that you can have”. Random and lovely – and saved me $2500.
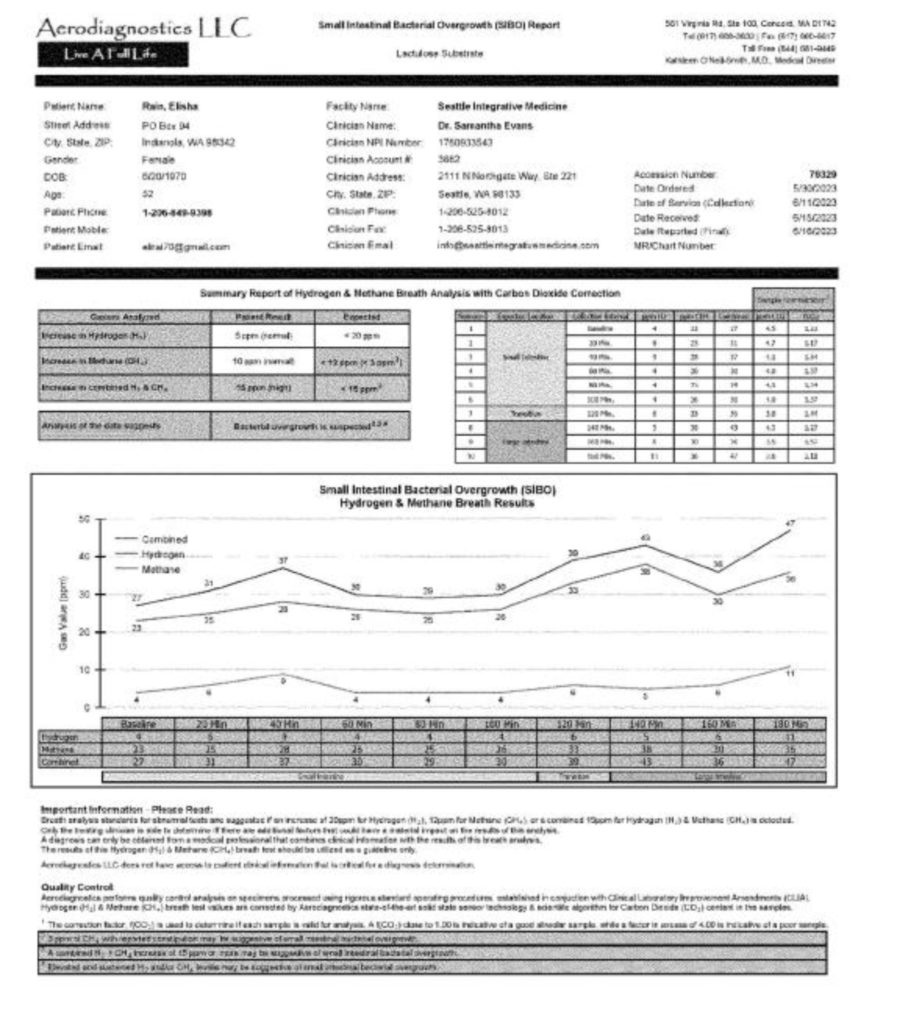
My frustration with the gastro doc was that he didn’t listen when I said (based on my extensive research and consistent with my symptoms) that I believe I have the form of SIBO known as “methane dominant” where I would need a second antibiotic (Neomycin) to be effective at eradicating the bacteria. He said that particular antibiotic wasn’t available due to a national shortage (turns out, not true). He also did not do the official SIBO testing (an involved three-hour breath test process) which would have confirmed (or ruled out) the methane-dominate variety.
To speed this story up, I did the antibiotics, and also reached out to my MS naturopath who referred me to a different naturopath in his practice with a lot of experience with SIBO. She ordered the breath test. which came back with a very clear SIBO positive, specifically methane dominant. The naturopath ordered another round of rifaximin and added it to the Neomycin which, it turns out, was very easy to get. I have now, as of yesterday, completed this cycle of treating this bacterial beast.
Right now, as I write this, I am filled with hope and excitement.
As the antibiotics started to do their work my energy has come back to a level I have not felt since May of 2022. My body is loosening up, the spasticity is so much better that I can’t quite believe I have lived as long I have this impacted. It’s possible that SIBO has been here at a low level for a lot longer than this last February. My body and life are coming back online.
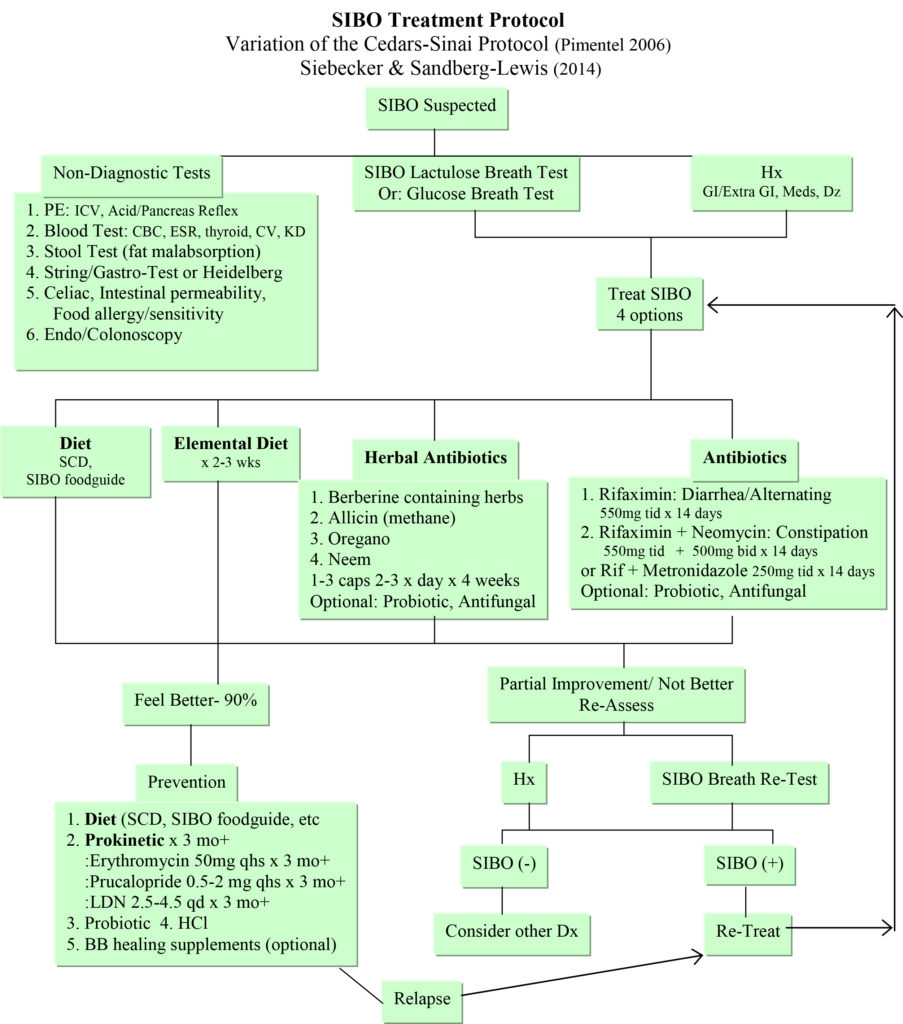
This round of treatment has not taken it all away, I can tell it’s not gone. I’m doing a second breath test today to figure out where I am now and will be on a very specific diet until those results come back, at which point we will consider next steps. The image I shared above shows the four main treatment pathways and we will figure out which one is next. It’s a long haul, but I’m totally fine with that because I can tell it is 100% worth it.
In the meantime, I bumped into a spoken word poet/artist, Andrea Gibson, who brought me to tears, made me smile, reverberated inside me as someone who has found a clear and loving voice inside of a very difficult personal world. Someone who has found the clearest connection to love in the face of death that I’ve ever encountered.
Here is a wonderful podcast with them.
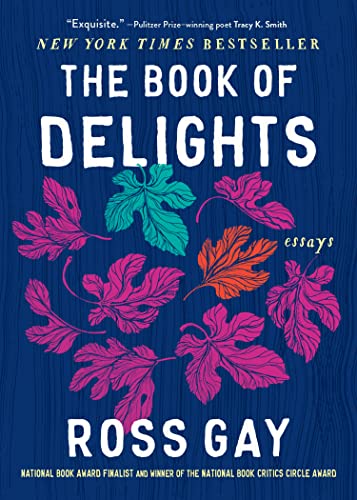
The day after bumping into Andrea Gibson, I heard a podcast with the poet/essayist Ross Gay whose focus is all about joy and delight. I’m just beginning to read his books, but his voice is infectious and a delight in its own right. His work is all about paying attention. I am learning that joy and delight can look like tears, can touch something that breaks open and bleeds.
So, I am reading and listening to poetry and audio books, re-reading my favorite Mary Oliver collection, reading Pema Chodron – digging into Buddhist philosophy, writing, meditating, researching, using music therapy to aid my PT, seeing a counselor. I have tried supplements, tried gut-directed hypnotherapy, tried to find delight, joy, and gratitude in the world, no stone unturned. Looking for ways to be at peace with pain if it doesn’t leave and doing everything in my power to usher it out.
Kira is home (along with her boyfriend Zac) for the summer, working on the farm across the street and I am soaking up this time with them – perhaps the last stint of living at home.

What I want to tell you is that I’m still here. I’m still on the riverbank with my toe in the water, soaking up life, connected to it enough. Craving a deeper dive, but proud that I’ve got that toe in at least. I can feel the vibrancy of life, I can still be brought to tears by a piece of poetry.






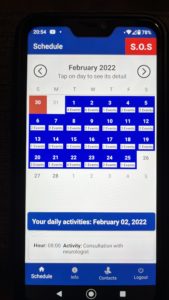
 For my own memory and for anyone else’s interest, I wanted to recount the four weekend monumental days that proceeded where I am now. All of this is written in a somewhat fatigue and chemo haze, so again mostly clinical not so poetic.
For my own memory and for anyone else’s interest, I wanted to recount the four weekend monumental days that proceeded where I am now. All of this is written in a somewhat fatigue and chemo haze, so again mostly clinical not so poetic.